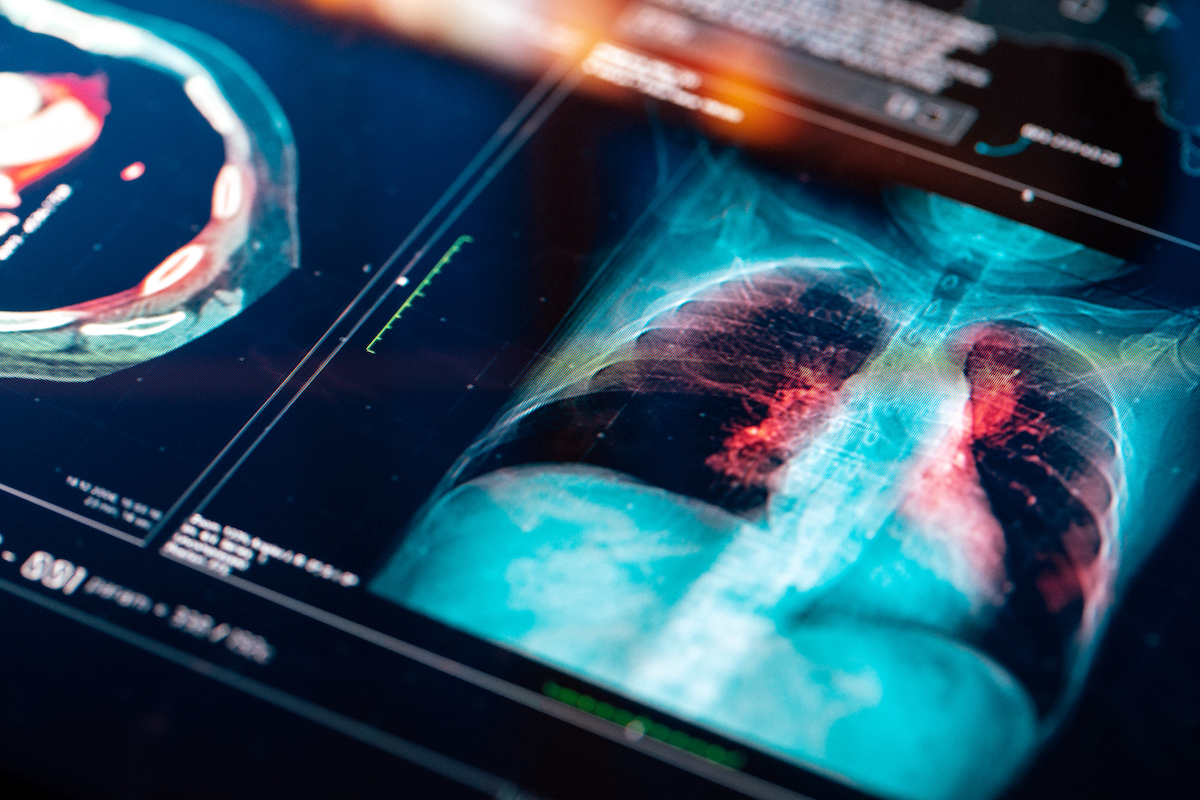
Determining how SARS-CoV-2, the virus causing COVID-19, moves from an early stage of infection, when patients are largely asymptomatic, into a later stage when people may experience life-threatening inflammation in the lungs, is a critical step in understanding how to target and treat the disease more efficiently. But that transition process is complex and cannot be easily studied as it happens in the human body.
Using a lab model they adapted from a model previously developed to study cystic fibrosis, a genetic disease affecting the lung, Emory researchers were able to replicate this complex interaction. In doing so, they identified the key immune cell type that drives the transition from early to late COVID-19 and were able to test candidate drugs on those cells, demonstrating their impact on viral clearance and inflammation.
The results of this new research are now in print and online as an open access article in Cell Reports. The study concludes that lung-infiltrating monocytes (a type of immune cell that can migrate into tissues) drive the development of inflammatory complications in COVID-19 and are a critical target for treatment. Furthermore, the study details how the anti-viral drug remdesivir and the immunomodulator baricitinib can be used alone or in combination to target those monocytes.
“SARS-CoV-2 really throws a wrench in the way the immune system works. Severe cases show a dysfunctional immune response and, unfortunately, we don’t fully understand why some patients are susceptible to that severe response and others are not,” says senior author Rabindra Tirouvanziam, PhD, immunologist and associate professor in the Department of Pediatrics at Emory University School of Medicine. “Our study answers an unmet need by mimicking this process in vitro and seeing how treatments might be used to prevent some of the worst effects of the disease, thereby improving patient outcomes.”
Importantly, the study documents that data obtained through the lab model mirror in vivo data gathered from hospitalized COVID-19 patients. Since the transition process is very difficult to observe in patients, this research provides a missing link of information and a way to better understand how and when COVID-19 treatments may work best.
The model used in the study mimics the sequence of events that happens when a person is infected with the COVID-19 virus. It is based on growing human epithelial cells that line the lungs with their top part exposed to air. These cells are then infected with SARS-CoV-2 and the model allows blood monocytes to transmigrate across the infected epithelium, where they acquire the virus. Anti-COVID-19 drugs can be added at any point to measure how they affect infection and immune response in epithelial cells and lung-infiltrating monocytes at different stages.
In the early stage of SARS-CoV-2 infection, the virus replicates rapidly but actively avoids attracting “first responder” immune cells — called “neutrophils” — which can initiate early inflammation and clearance of the virus. The infected person doesn’t develop symptoms and, in fact, might replicate and then clear the virus without ever experiencing any symptoms. But eventually, monocytes also respond; these immune cells live longer than neutrophils and can also transmigrate into the lungs to acquire the virus and copy its genetic template, which tells the body to escalate its immune response. It is precisely that escalation that can trigger an excess of inflammation.
“The escalation is the problem,” says Tirouvanziam. “There may be little to no live virus left but the lung-infiltrating monocytes will acquire and replicate its sequence and keep the immune response going, so inflammation is persistent and may rapidly build up.”
The study found that the combined use of two FDA-approved treatments for COVID-19 — remdesivir and baricitinib — enhances antiviral signaling and viral clearance by the monocytes infected with SARS-CoV-2. It highlights the timing of therapeutic treatments as critical to heading off severe inflammation, which can lead to the life-threatening condition known as acute respiratory distress syndrome.
The small airway model in this study is unique in that it uses human cells in a system mimicking the lung environment. Tirouvanziam says this is an ideal platform for testing more drugs against SARS-CoV-2 variants. “It’s important to note that this is not over. There are new variants constantly arising, and for the foreseeable future we’re going to be exposed to these probably several times a year. There’s an urgent need to keep developing and testing drugs to efficiently counter these variants,” says Tirouvanziam.
The Tirouvanziam lab collaborated with the Schinazi lab (division of biomedical pharmacology within Emory pediatrics), the Ghosn, Sukhatme and Bhasin labs, also at Emory, and the Gibson lab at Georgia Tech to implement this study. It was supported by a National Science Foundation EAGER Award (https://www.nsf.gov/awardsearch/showAward?AWD_ID=2032273) and an internal Woodruff Health Sciences Center COVID-19 CURE Award.