Cancer cells are not interested in sustainability. They gobble up sugar inefficiently, brushing aside their mitochondria, the efficient miniature power plants that supply energy to healthy cells.
Researchers at Winship Cancer Institute, Emory University have identified an important control switch used by cancer cells to tune down mitochondria and ramp up growth under conditions when oxygen is limited.
Scientists led by Jing Chen, PhD, have identified an enzyme involved in the control switch, ACAT1 (acetyl-CoA acetyltransferase) as a potential anticancer drug target.
The results were published recently in the journal Molecular Cell. Chen is associate professor of hematology and medical oncology at Emory University School of Medicine and Winship Cancer Institute. Co-first authors of the paper are instructor Jun Fan, PhD, postdoctoral fellows Changliang Shan, PhD, and Hee-Bum Kang, PhD.
Co-authors at Winship include hematology and medical oncology faculty Sagar Lonial, MD, Manila Gaddh, MD, Martha Arellano, MD, H. Jean Khoury, MD, Fadlo Khuri, MD and Sumin Kang, PhD. Collaborators at Cell Signaling Technology contributed to the paper.
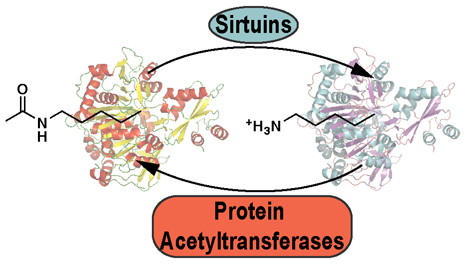
The findings highlight how acetylation – a chemical modification of a protein, potentially changing its function -- on key metabolic enzymes pushes cancer cells’ rapid growth.
“Much of the investigation of how cancer cells’ altered metabolic enzymes are regulated has emphasized another chemical modification: phosphorylation,” Chen says. “We are finding that acetylation may play an equally important role, and that metabolic enzymes’ acetylation presents opportunities for anticancer drug development. ACAT1 is one of the first examples of a protein acetyltransferase in mitochondria.”
Cancer cells tend to turn down their mitochondria in favor of a more inefficient mode of using glucose called glycolysis. This phenomenon is known as the Warburg effect, named after 1931 Nobel laureate Otto Warburg. Cancer cells benefit from this metabolic distortion because the byproducts of glycolysis can be used as building blocks for fast-growing cells.
Chen and his colleagues were focusing on the enzyme pyruvate dehydrogenase. Acting as a sort of control valve, pyruvate dehydrogenase governs how much fuel is sent through mitochondria. Pyruvate dehydrogenase is found in mitochondria in a complex with several other related enzymes.
Chen’s team found that in many types of cancer cell lines (lung, head and neck, breast and several types of leukemia), two parts of the pyruvate dehydrogenase complex are acetylated, but these modifications are less abundant in healthy cells.. These modifications were also found in normal cells stimulated to proliferate by a growth factor involved in cancer signaling (epidermal growth factor), and in samples from patients with acute myeloid leukemia.
Chen’s team showed that acetylation of PDHA1 (pyruvate dehydrogenase) and PDP1 (pyruvate dehydrogenase phosphatase) help cells grow in conditions of limited oxygen, which cancer cells often face because they grow faster than their blood supply.
They identified the enzymes that carry out acetylation (ACAT1) and the reverse reaction, deacetylation (SIRT3) on the pyruvate dehydrogenase complex. In addition, they found that “knockdown” of ACAT1 in human cancer cells resulted in reduced tumor growth when the tumors are grafted into mice. ACAT1 has previously found to be elevated in several types of cancer and thus could be an anticancer drug target, Chen says.
However, prolonged inhibition of ACAT1 could lead to ketoacidosis, since a genetic deficiency in ACAT1 in humans causes ketoacidosis; more investigation of the consequences of systemic ACAT1 inhibition are needed, he says.
The research was supported by the National Cancer Institute (CA140515, CA116804), the Department of Defense (W81XWH-12-1-0217), the Samuel Waxman, Max Cure and V Foundations and the Georgia Cancer Coalition.
Reference: J. Fan et al. Tyr Phosphorylation of PDP1 Toggles Recruitment between ACAT1 and SIRT3 to Regulate the Pyruvate Dehydrogenase Complex. Mol Cell. 53, 1-15 (2014).